France announced last month a new case of bovine spongiform encephalopathy (BSE), popularly known as “Mad Cow Disease,” in a four year old female cow. This is the first case of this type of BSE in France since 2011, but follows on the heels of two other cases in Europe just last year, one in Ireland and the other in Wales. BSE cases are very rare today, but the French case raises some interesting, and slightly disturbing, questions.
BSE is caused by the abnormal folding of a type of protein, called a prion, which is common in nervous tissues of cattle, humans, and other animals. Much remains to be learned about this process, and some speculate that a virus or bacteria may be involved in catalyzing the transformation of normal prions. But no good candidates have been found so far.
When these abnormal prions interact with normally-folded prions, the latter also become abnormal. The misshapen proteins grow in number, creating cavities that give a characteristic “spongy” appearance to the brain under a microscope. As the abnormal prions are made by the affected animal’s own body, the immune system mounts no response, making it difficult to diagnosis BSE prior to death.

A normal prion protein (left) with an abnormally folded prion protein (right), present in animals bovine spongiform encephalopathy. Part of the normal helical form of the amino acids transform into fibrous sheets (arrows) in the abnormal form. Creationwiki
From the time abnormal prions begin to form in cattle, it typically takes anywhere from 2 to 8 years for clinical signs to appear. These include abnormal walking, tremors, aggressive behavior, and/or weight loss, followed by inability to stand, coma, and death usually within six months of the first signs of illness.
Where did BSE Come From?
BSE was first recognized in UK cattle in 1984-86, though cases may have been present as early as the 1970s. The disease spread throughout the UK and, to a limited extent, in a few other countries, peaking in 1993 with around 1000 BSE cases reported each week.
It was hypothesized that BSE occurred when cattle consumed meat and bone meal (MBM), a common feed supplement, contaminated with abnormal prion proteins from slaughtered cattle with BSE. These prions proved highly resistant to heat, ultraviolet and ionizing radiation, and other procedures that were hoped might inactivate the prions in feed. As a result, in 1988 the UK government banned the use of proteins originating from cattle or any other ruminants (particularly sheep and goats) as an ingredient in all ruminant feeds.
This protein feed ban had the intended effect. After more than 37,000 BSE cases in the UK in 1992, the incidence fell steadily over the coming years, to fewer than ten per year by 2011. By the time the situation was under control, over 184,000 BSE cases had occurred in the UK and another 6000 or so elsewhere in the world. These affected Ireland, France, Portugal, Spain, Germany, and Switzerland most, though Canada (18), the US (4), and Japan (37) have each had a few cases, often related to cattle imported from the UK.
BSE cases outside of the UK, however, did not peak until 2002, a full ten years after the UK peak. This may be partly due to the UK’s policy of exporting to other countries its banned MBM and other animal products, with little or no warning that they may have contained prions that cause BSE.
Humans: Cannibals and other Carnivores
BSE was a big deal when it was identified in 1986. But it would not have attained the media attention it did had the disease not begun to cause disease in people too. No human cases were known early on, but when a few cats fed BSE-contaminated food acquired the disease and died, speculation emerged that people may be able to acquire BSE in the same way. As a precaution, in 1989 cattle tissues in which prions may be found (brain, spinal cord, spleen, thymus, tonsils, and intestines) were banned from human foods. But it was too late for some. The first cases of the disease in people began to appear in the mid-1990s.
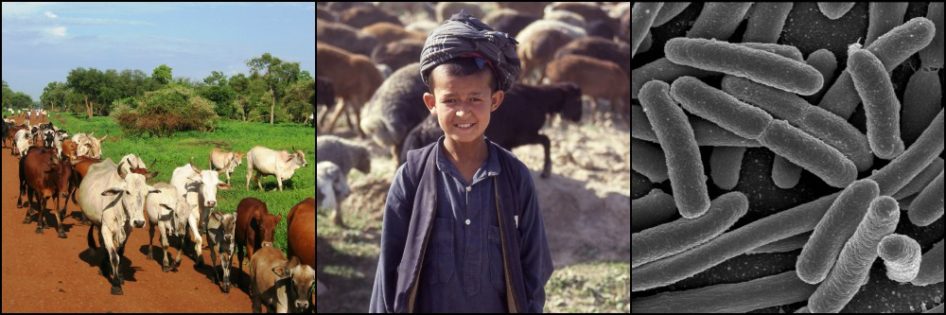
Humans (along with several other mammal species) have long had their own forms of prion disease very similar to BSE in cattle. One is called Creutzfeldt-Jakob disease (CJD). As with cattle, one way of getting CJD is consuming contaminated tissue, in particular brain, from an affected person. Some societies practicing cannibalism, such as the Kuru people of New Guinea, lost up to 1% of their population to CJD each year. They have now stopped the ritualistic consumption of their dead that spread the disease.
Yet CJD occurs occasionally in non-cannibalistic peoples too. This “sporadic” form of CJD seems to affect about one person in a million around the world each year, and the spark that leads to abnormal folding of the victims’ prions is unknown.
In 1995, when two teenagers and a woman in her 20s were diagnosed with CJD in the UK, alarm bells sounded. “Sporadic” CJD typically occurs in people over 60 years of age, and almost never in those under 40. Other aspects in these and other new patients were also different. While behavioral changes such as depression, anxiety, and hypersensitivity to pain appeared similar to the sporadic CJD, neurological symptoms demonstrated a later-than-expected onset, and included difficulty walking and talking, tremors, and dementia. And patients lived with their symptoms on average for just over a year before death occurred, much longer than the 4-5 months of sporadic CJD patients. It was strongly believed that these recent cases resulted from consumption of foods contaminated with BSE. This new form of CJD was dubbed variant CJD, or vCJD.
I lived in France in the 1990s when these first human cases occurred in the UK, and soon afterwards in France. Rumors ran wild and many people were convinced the disease would end up killing millions of people within a few years. Fortunately this has turned out to be unlikely.

Progression of prion diseases Source
vCJD peaked in the UK in 2000 when 28 cases were reported, then steadily declined to zero in 2012. In total, 229 cases including 27 in France and five or fewer cases in ten other countries have occurred to date. This compares to an average of 63 cases of “sporadic” CJD every year in the UK alone. So BSE-induced CJD, even at its worst, did not affect nearly the number of people that sporadic CJD does.
Sporadic Cases Continue
I mentioned for a reason the age of the cow recently diagnosed with BSE in France. She was born in 2011, more than a decade after France banned the incorporation of meat and bone meal in ruminant feeds.
Similar to humans, cattle also have a form of BSE that is so rare it is considered to be “spontaneous” in nature and does not require consumption of BSE-contaminated feed. However this possibility was dismissed in the recent French cow when her abnormal prions were tested and shown to be incompatible with this form of the disease (one such case, however, was found in France in 2014).
The French are considering 4 explanations in this recent case:
- BSE-contaminated tissues somehow made it into the animal’s feed (considered highly unlikely given the long-standing ban on animal proteins in ruminant feed)
- Vertical transmission of BSE, i.e. from mother to daughter in this case (considered very unlikely in that vertical transmission of BSE has been suspected in only a very few cases and never proven, and given that the mother in this case was slaughtered in 2015 with no signs of BSE)
- The existence of an unidentified form of “spontaneous” BSE that closely resembles the form of BSE thought to be induced by consumption of BSE-contaminated feed (possible, but very difficult to prove)
- A genetic predisposition of the cow to acquire BSE (only one such case has been identified before)
The mystery behind this recent case of BSE in France may never be answered. And there will be other isolated BSE cases posing similar questions. In the meantime, France will await to see if its international status as a country with “negligible BSE risk,” obtained only 7 months ago, will change, leading to potential trade restrictions.
References
Baron, T., Biacabe, A-G., Calavas, D. (2016). Un Cas d’ESB classique chez un bovin né en 2011. Plateforme ESA.
“Bovine Spongiform Encephalopathy.” Technical Fact Sheet. Center for Food Security and Public Health, May 2012.
Collinge, J. (2008). Lessons of kuru research: background to recent studies with some personal reflections. Phil. Trans. R. Soc. B., 363, 2689-3696.




I found this very interesting as my uncle died of a variant of CJD in 1996. The variant was called pics disease I believe. He was studied at Yale as he lived in CT. No one could figure out how he got it, but the family has an interesting theory. Being of Italian immegrant parents he ate something called Soffritto that his family made. This was a stew made with cows ” organs” such as brain, lungs, hearts etc. along with pork sausage and vegetables in a tomato base. Kind of a stew, but often put in a big roll and eaten like a sandwich. My mother (his sister) wouldn’t eat it but continued the tradition of making it for my father and her brothers that did. I remember when they “couldn’t get” organs anymore and she switched to just hearts which she could still obtain. Her brothers sometimes made it with venison organs that they obtained by hunting. The family speculates this is where he picked up the virus. Is it in deer?
No one else has shown any signs of this horrible disease, but we have been stopped from giving blood when we answer yes to the question of a relative with CJD. I’ve told them it was a variant and he was my uncle not immediate family, but they turned me away to be safe so never tried to donate again. Anyway, thought that history of them consuming organs as an Italian dish might be of interest.
That is very unfortunate about your uncle. I’m sorry.
It is interesting that he became ill just as the first BSE cases were appearing in the UK. Nothing is impossible, but from what you describe, this seems to likely be a coincidence only.
I know little about Pick’s disease but, as you suggest, it causes behavioral changes similar to those of CJD. As I understand it, Pick’s disease is caused by an abnormal accumulation of proteins in the brain, but NOT of prion proteins. An autopsy would presumably have confirmed the diagnosis.
Deer species in North America have their own type of prion disease, called chronic wasting disease. It was discovered in 1967 in Colorado and spread slowly but steadily over the next 4 decades (Europe declared their first case of CWD ever in the past couple of weeks – a reindeer in Norway). I believe it wasn’t until the 2000s that CWD was found in East Coast deer, making it too late to explain your uncle’s disease. Hunters are warned to take precautions when butchering and eating deer, but I don’t think there have been any cases, even suspected, of a human getting CWD. In fact, the bovine form (BSE) is the only one that seems able to cross into distantly related species (people, cats…) under natural conditions.
Thank you for your reply and this interesting new information. I will tell the family.