The northeast coast of Colombia, focus of several major Venezuelan equine encephalitis outbreaks in people and animals. Charles Hoots
After a trip to Colombia last November, I wanted to do a post on Venezuelan equine encephalitis (VEE), yet another zoonotic, mosquito-borne virus of the tropics. The northeast coast of Colombia, along with neighboring Venezuela, has been the focus of several outbreaks of VEE in the past. But the last major one occurred in the 1990s and I decided it wasn’t current enough to write a post on.
Right on cue, in December 2016 Colombian authorities announced a mass equine vaccination campaign and restrictions on horse movements into and out of Colombia’s Cesar Department in response to an as yet limited VEE outbreak there. Colombia’s caution is warranted, given the unpredictable nature of this disease that in the past has vanished for decades at a time, only to reappear with devastating effects just when it was about to be written off as gone forever.
Background
VEE virus occurs only in the Americas and is in fact a group, or complex, of 6 similar but distinct virus subtypes (I-VI). Many, if not all, occasionally cause flu-like symptoms in people, but only subtype I can lead to widespread mass disease in people – called epidemics – and in equines (including horses, donkeys, and mules) – called epizootics. In the remainder of this post, “VEE virus” will refer to subtype I only, unless otherwise stated.
VEE virus was first discovered in the 1930s, though the earliest outbreaks were retrospectively identified from the 1920s. The virus strains circulate constantly between rodents and mosquitoes (and possibly birds) living in humid forests and swamps, rarely emerging from these strongholds.
For 50 years from its first appearance, widespread outbreaks of VEE in horses and humans occurred on average every 10 years or so in high risk regions of South America. Horses, donkeys, and mules become ill with fever and depression for 4-5 days. This is often followed by signs of encephalitis (brain inflammation) such as circling, incoordination, and excitability. Well over half of these animals typically die within a week of encephalitis onset, resulting in the deaths of thousands, even tens of thousands of equines during these events.

Map showing areas of common Venezuelan equine encephalitis outbreaks in the past (in red) and table of large VEE outbreaks. Note the preponderance of I-AB serotype up to 1973, and its apparent disappearance since then (see text for explanation).
It was only in the 1950s, in Colombia, that the connection was made between these equine epizootics and human illness. A large percentage of people in outbreak areas suffered simultaneous cases of fever, headache, and muscle pain. In about ten of a hundred of these cases, neurological symptoms develop soon afterwards, including convulsions, confusion, drowsiness, and sensitivity to light. Of these neurological cases, one in ten may die and a few others, particularly children, may suffer permanent neurological damage.
Equines as Amplifiers
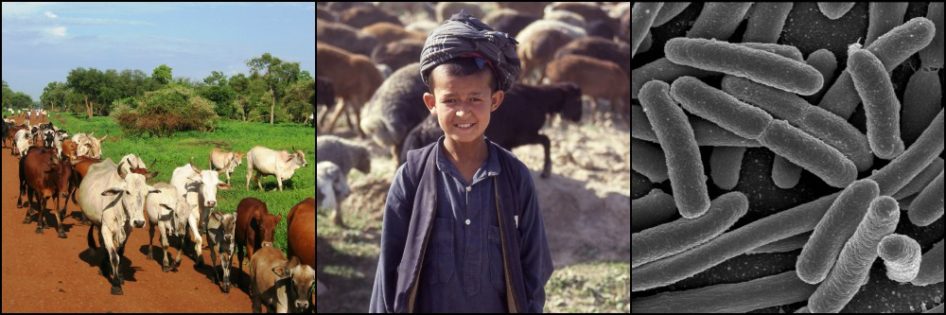
When VEE epizootics occur, equines suffer such high incidence (infection) rates, and virus reaches such elevated levels in their bloodstream, that the disease easily spills over into nearby humans, transported by those mosquito species that feed on both equines and humans.
People also have high virus levels in their blood but they apparently are not the favored food source for the most efficient mosquito species vectors and so act for the most part as dead-end hosts. Sheep, cattle, pigs, dogs, bats, rodents, chickens and some other bird species are also susceptible to VEE virus infection, however no epidemic (i.e. in humans) is known to have occurred in the absence of simultaneous widespread infections in equines. This is why VEE is not a factor in urban areas, where people are densely packed but there are no equines to “amplify” the virus.
But in rural areas the effects can be devastating. In a 1969 outbreak in Ecuador, VEE was reported in 31,000 people, 310 of whom died from the disease, while 20,000 equines also perished. Two outbreaks in Colombia and Venezuela during the 1960s resulted in an estimated 200,000 human VEE cases and more than 100,000 equine deaths.

Transmission cycles of Venezuelan equine encephalitis virus. “Enzootic” is the animal equivalent of “endemic”, meaning the virus circulates at low levels, causing little harm in its hosts. The dashed arrow linking the two cycles represents the mutation of the I-D serotype to I-AB or I-C, allowing the virus to spread rapidly between equines and people. USDA APHIS
Disappearing Act
Then something strange happened. In 1969, VEE outbreaks expanded out of South America for the first time, going on a three-year rampage through Central America and Mexico, reaching as far north as Texas. 50,000 equines died and a similar number of human VEE cases were reported.
After this outbreak fizzled out in 1972 and another in Colombia/Venezuela the following year, inexplicably VEE epidemics and epizootics disappeared for two decades. Speculation abounded as to whether the virus variants causing the disease were gone forever.
But in the 1990s, VEE returned from the dead with a vengeance.
The Quest for Answers
The behavior of VEE left many unanswered questions. For example, if VEE outbreaks occurred every 10 years or so in a particular area, where did the virus that causes the disease hide out in the interim?
Work on the subtype I virus known to cause VEE resulted in the classification of 5 distinct variants – referred to as I-AB, I-C, I-D, I-E, and I-F, each differing slightly from the other in genetic make-up. In all VEE outbreaks in equines and people up to 1992, either the I-AB or I-C variant was implicated as the cause (see embedded Table in map above).
But when outbreaks ended, sampling in the affected areas revealed for the most part only the I-D variant, circulating most conspicuously in rodents inhabiting nearby forests and swamplands. Little or no I-AB or I-C was to be found. It was as if these variants appeared spontaneously every decade or so.
Improved laboratory techniques soon led to the discovery that the I-AB and I-C viruses both differ from the I-D variant in just a handful of the 11,400

Portrait of a single-stranded RNA virus similar to the various Venezuelan equine encephalitis viruses. The orange strand in the center represents the viral genome. Bedford
nucleotide bases making up their RNA genomes (we have seen in previous posts how RNA viruses are especially susceptible to mutations). Of these few base mutations in I-AB and I-C, one that is always present results in a change in only one, sometimes two, amino acids within the long chain of amino acids making up the E2 glycoprotein.
The E2 glycoprotein is found in the virus envelope and plays a crucial role in binding to host cells of infected animals. This tiny alteration is enough to significantly increase the virulence of VEE in equines and people, which consequently greatly increases the amount of virus in their blood streams.

An example of a small portion of the more than 11,000 nucleotide bases making up the single RNA strand in each VEE virus. Each group of 3 bases (called a codon) produces a specific amino acid when translated inside an infected host cell. Hundreds to thousands of these amino acids join in a chain to form proteins. The change in just one specific nucleotide base can cause a change in a single amino acid, allowing the virus to infect and sicken thousands of people and equines. Splettstoesser
Putting the Pieces Together
These discoveries have given us a much better understanding of VEE epidemiology and ecology. The story, using the northeastern Colombia/Venezuela VEE focus as an example, goes something like this:
- In “normal” times, the I-D variant of VEE virus is transmitted at relatively low levels by Culex mosquitoes between rodents in swamps and forests.
- Occasionally genetic mutations lead to the substitution of one or two nucleotide bases coding for the E2 glycoprotein of the I-D virus, transforming it into either an I-AB or I-C variant.
- If picked up by competent mosquito vectors (e.g. various Psorophora, Aedes, Mansonia, and Deinocerites) that subsequently feed on a susceptible horse, donkey, or mule, VEE disease can explode through the population.
- Because they feed many more mosquitoes than can a rodent, equines fuel, or ”amplify,” the spread of the virus to other susceptible equines and also to people. Even mosquitoes that are not particularly good transmitters of the virus play a role because of the high virus levels in so many affected equines.
- Only when the great majority of equines in the area have been infected does the virus die out, with nowhere else to go. Unlike the I-D variant, I-AB and I-C do not spread well in rodents and so probably cannot (or rarely) retreat to the forests and swamps to bide their time.
- With the death of old equines and their replacement by offspring or imported animals, immunity declines within a few years and a new naïve population becomes susceptible to another outbreak. This is why major outbreaks fail to occur more frequently than about 5 years in the same place. It takes time to replenish the naïve population.

Certain rodents in forests and swamps are commonly infected with the VEE virus I-D serotype by Culex spp. mosquitoes. These hosts either show no signs or are slightly ill for a few days only. But several develop high levels of the virus in their bloodstream, facilitating transmission to feeding mosquitoes. When the I-AB or I-C serotypes develop from this population, these viruses abandon the rodents to focus on equines and people. VEE outbreaks in Colombia and Venezuela are often associated with populations of the Boyacá spiny rat (Proechimys chrysaeolus), similar to the Proechimys rat in this photo. Carlos Boada
The Demise of I-AB
Another VEE enigma is that all but one of the approximately 15 major VEE outbreaks between the 1920s and 1973 were caused by the I-AB variant, with the remaining one due to I-C. However, since the 20-year absence of VEE epizootics that began in 1973, no I-AB variant outbreaks of VEE have occurred.
Given the high mutation rate of RNA viruses, researchers were surprised to find that the I-AB variant implicated in several of the mass outbreaks in the 1960s and 70s was almost identical genetically to viruses isolated from outbreaks in the late 1930s.
The severity of VEE had led to the development and widespread use in the 1940s of an inactivated (i.e. killed virus) vaccine using the I-AB variant. This sparked speculation that viruses from the 1930s used in making the vaccines occasionally failed to be inactivated by the vaccine production process. This may have exacerbated, or even caused, one or more of the epizootics through the 1970s.
Another possible explanation is that the I-AB variant kept a low profile between outbreaks during those 40 years, circulating at very low levels in some unknown host animal. But, again, scant evidence for this has been found.
With the development of a safer, better, live attenuated vaccine (i.e. live virus whose virulence has been diminished) in 1961, the old I-AB based vaccine was phased out of use during the 1969-72 VEE outbreaks. No epizootics since that time have been caused by the I-AB variant, supporting the hypothesis that the old vaccine may have been partly to blame.
Only the I-C variant returned after the 20-year hiatus, causing two separate mass outbreaks in Colombia/Venezuela in the 1990s. Since then, numerous relatively small variant I-C outbreaks have occurred from Guyana through Central America to Belize, affecting sometimes just a few dozen equines and even fewer people. Is this the new norm? Or are we simply overdue for another mass VEE outbreak?

Wayuu courtship dance. The indigenous Wayuu people of NE Colombia and NW Venezuela inhabit one of the areas hardest hit by VEE outbreaks in the past. They owned many of the estimated 70,000 horses, donkeys, and mules affected by the 1995 VEE outbreak on Colombia’s La Guajira Peninsula. Herds of feral equines, impossible to vaccinate, have complicated control of outbreaks there. Tanenhaus
The Future
We might be tempted to believe that VEE epizootics and epidemics are now fewer and farther between given the apparent elimination of I-AB variant. That may be too optimistic.
Firstly, though vaccination of equines can control and even prevent VEE outbreaks, the long periods between these outbreaks inevitably results in complacency among animal owners and governments to keep up with vaccination schedules. This eventually leads to a large susceptible population of equines ripe for infection when the circumstances are right again.
Secondly, if this blog shows little else, it is that Nature has a way of doling out the unexpected. For example, in 1993 and again three years later, for the first time VEE virus variant I-E caused illness in over 150 equines in southern Mexico, leaving half of them dead. Similar to the I-AB and I-C variants, this virus likely results from a mutation in possibly just a single nucleotide base. Long-time VEE researcher Scott Weaver says this new virulent I-E variant did not produce high enough virus in the blood to allow efficient transmission by mosquitoes and so did not spread far. But, Weaver believes, “presumably this I-E strain still circulates in southern Mexico,” remaining under the radar for now.
The various members of the Venezuelan equine encephalitis group of viruses circulate from Argentina in the south to Florida and the Rocky Mountains of the US in the north. Believe it or not, the issues covered superficially in this post are but the tip of the iceberg of VEE’s complexities.
We are learning that these viruses, once thought to be for the most part benign, may cause much more common human illness than was previously believed, being frequently misdiagnosed as dengue fever infections in particular. Changes to RNA viruses like VEE virus occur suddenly and with unpredictable consequences. The near elimination of I-AB variant as a problem will not be the end of the story.
References
Aguilar PV, Estrada-Franco JG, et al. Endemic Venezuelan equine encephalitis in the Americas: hidden under the dengue umbrella. Future Virol. 2011: 6(6): 721-740.
Anishchenko M, Bowen RA, et al. Venezuelan encephalitis emergence mediated by a phylogenetically predicted viral mutation. Proc Natl Acad Sci USA. 2006; 103(13): 4994–4999.
Weaver SC, Ferro C, et al. Venezuelan equine encephalitis. Annual reviews, entomology. 2003; 49: 141-174.
US Dept of Agriculture, APHIS, Veterinary Services. Venezuelan Equine Encephalomyelitis Standard Operating Procedures: Overview of Etiology and Ecology. 2013 Aug. Foreign Animal Disease Preparedness & Response Plan.