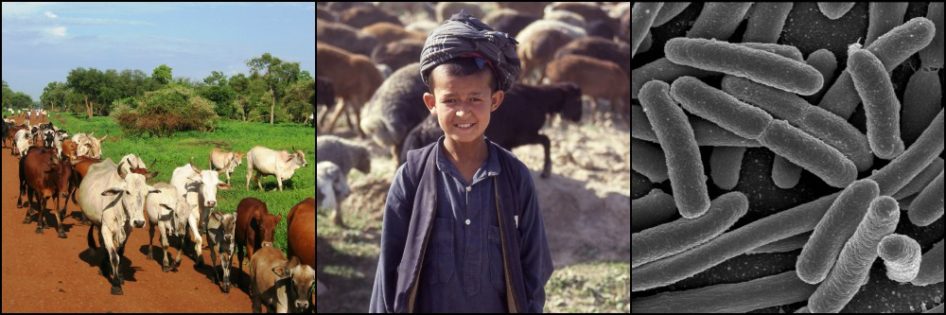
Villagers in Uganda bringing their chickens for avian influenza testing, 2009 Stephanie Smith
We don’t hear much any more about fears of an avian influenza pandemic sweeping the world. But the unique characteristics of avian influenza viruses and their expanding global presence make them as likely as ever to acquire the ability to thrive in people. This post and the next explain why these viruses are different and what can – and cannot – be done to stop them.
The outbreak of avian influenza in the US state of Indiana on 14 January, following on the heels of a much larger outbreak the previous year, reminds us of the “bird flu pandemic” that didn’t happen. As prominent in the news a few years ago as Zika virus is today, an avian influenza pandemic in humans remains a grave concern, and for good reason. In public health as in investing, “Past performance does not guarantee future results.”
As a veterinary student, I spent the summer of 2009 working in southwestern Uganda. Among other activities, I sampled chickens in rural areas for avian influenza viruses using test equipment and funding provided by the US government. In the villages where we sampled, cattle are kings and families were embarrassed to admit to us that they kept poultry, as though it indicated their cattle were not enough for them. Only when the Ugandan veterinarian with us donned the white, head-to-toe biosecurity Tyvek suit provided with the testing kits did people begin bringing their chickens to us for sampling. The suit proved that chickens could be taken seriously.
Still, Uganda had suffered no serious avian influenza outbreaks up to then, and I remember thinking the money could have been better spent on more common diseases ravaging the country. Only later did I understand that monitoring for avian influenza is not just about keeping poultry healthy, but humans too.
What is Avian Influenza?
Avian influenza (AI) viruses adapted to wild birds long ago. The viruses are widespread but rarely cause overt illness in wild birds, a good indication that pathogen and host have evolved together over many generations and come to a mutual understanding of sorts.
AI viruses are classified in many ways, but one of the more common classifications uses two proteins located on the outer surface of the virus. The first protein, hemagglutinin, assists the infectious viral particle, called a virion, in attaching to and penetrating host cells in a bird. The second protein, neuraminidase, helps a new virion exit the host cell in which it was produced, allowing it to infect other cells.
18 different types of hemagglutinin (H, for short) and 11 types of neuraminidase (N) proteins are known. Every AI virion contains one of each in any of 198 (i.e. 18 x 11) possible combinations, generating such names as H5N1, H7N9, H3N3….

Structure of an avian influenza virion. Note the hemmaglutinin and neuraminidase on the outer surface and the 8 segments containing the RNA genome (nucleoproteins) in the interior. ViralZone
AI viruses can wreak havoc in crowded flocks of domestic poultry, from chickens and turkeys to quail and sometimes domesticated geese and ducks. The virus spreads rapidly, causing varying degrees of illness including lethargy, loss of appetite, and reduced egg production. These are called low pathogenicity avian influenza (LPAI) viruses because they do not kill large numbers of birds.
The problem is that these relatively mild LPAI viruses, once in a domestic poultry flock, can change into a much deadlier (pathogenic) virus, called highly pathogenic avian influenza (HPAI) virus.
How does the virus change?
When the cells of humans divide and multiply, they copy each of the 3 billion nucleotide base pairs making up their strands of DNA. Mistakes are occasionally made, but specific enzymes act as a proofreading mechanism and only 1 mistake (called a mutation) per 10 billion base pairs makes it through. This gives essentially identical strands of DNA in the daughter cells.
Avian influenza viruses, on the other hand, use RNA rather than DNA to store their genetic material. And RNA viruses lack the proofreading enzymes that prevent copying mistakes. The result is an average of one error for every 10,000 nucleotide bases reproduced. With only around 14,000 nucleotide bases making up the entire AI virus genome, that comes to almost one mutation for each new virion produced. It doesn’t sound like much, but it adds up when billions of virions are involved.
As if that weren’t enough, the genetic material of each AI virion is divided into 8 distinct segments. When more than one influenza virus infects the same cell, they often exchange one or more gene segments in a process called reassortment. Abrupt changes can follow.
Most mutations and many reassortments have either little effect on or are harmful to the virus. But occasionally they result in the virus causing severe illness and very high transmission rates in domestic poultry. This marks the transition from a low pathogenicity to a highly pathogenic AI virus. The latter can run through a poultry flock in no time, often killing 90% or more of the birds.
About 20 years ago, some of these highly pathogenic avian influenza (HPAI) viruses started causing illness in people who were in prolonged contact with infected birds. Most suffered only conjunctivitis (eye infections) or mild respiratory symptoms. However – and this is the bad news – a highly pathogenic H5N1 virus discovered in southern China in 1996 sent 18 people to the hospital, with 6 of them dying from the infection. That was the wake-up call, promptly responded to by the media.
The virus laid low until 2003, when it began to spread rapidly across Asia, Europe, and Africa. In addition to 100s of millions of dead poultry, 844 human infections with H5N1 were reported in 15 countries between 2003 and November 2015, including 449 deaths. Indonesia, Vietnam, and Egypt have been hardest hit. While concerning, these numbers are small when compared to the well-known seasonal flu, which kills 36,000 Americans alone every year and sends 200,000 to the hospital.
This particular H5N1 virus clearly does not spread easily from birds to people and even less so from person-to-person. Why? Because HPAI viruses invade host cells by binding to a specific receptor on the cell surface of their victim. Humans do not have this specific receptor. But a similar one is located on cells deep in the human respiratory tract, to which HPAI viruses occasionally bind. The few unlucky people to have acquired AI in nearly all cases had been around large numbers of infected birds, inhaling the virus deep into their lungs for prolonged periods. Infection leads to rapidly progressing pneumonia and death in 60% of patients.
With the AI virus genome’s ability to rapidly mutate and reassort, the fear is that such a deadly virus will adapt to the human cell receptors and bind them more easily. If this happens, the virus could spread more easily from person-to-person, much like the common cold, causing the much-awaited “bird flu pandemic.”

An example of genetic reassortment between two influenza viruses, in this case one human and one avian. Note how the 8 RNA genome segments in the new virus come from either the avian strain or the human strain, making a mixture of the two. Dhorspool at the English language Wikipedia
Viruses over time tend to minimize the amount of death and destruction they leave behind when adapting to a host. But the consequences for people could still be devastating in the short run.
What Has Changed?
Why is avian influenza threatening humans only now, when it has been around so long? Denser human, livestock (particularly pigs), and poultry populations play a huge role as mixing bowls for viruses to exchange genes. Wetland destruction crowds migratory birds into ever smaller areas, serving the same purpose. And the ease of international travel and trade helps spread the viruses and would be a major concern in the event of a pandemic.
Prevention and control measures are difficult. Making a vaccine against a virus that doesn’t exist yet is not very practical. And the rapid changes in AI viruses make the effectiveness of any vaccine short-lived, in the same way that seasonal flu vaccines for people must be different each year. Mutations and reassortment also make AI viruses masters at resistance to the few antiviral medications that exist.
The primary strategy, in the US and Europe at least, is to detect and eliminate all H5, H7, and H9 viruses in poultry, as these are the only virus types that have caused human illness so far. A major problem for this strategy is that these viruses start out as low pathogenicity viruses and may circulate for weeks or months before they are detected, since they don’t always make infected poultry sick. But catching them early is critical. That explains why I was busy collecting chicken samples in Uganda at a time when avian influenza was hardly known in that country.