Space-fill drawing of a whole Zika virus particle, and a cross-section as it interacts with a cell. The outer capsid is pink, the membrane purple, and RNA genome in yellow. Cell-surface receptors are green, cytoskeleton blue, and blood plasma gold. David Goodsell
Zika virus is one of a large number of viruses transmitted between animals (including humans) by arthropod insects. These are called arthropod-borne viruses, or arboviruses for short. The arthropod vectors in the case of Zika virus are certain mosquito species that transmit the virus from one host to another. But arboviruses also require a reservoir host: one or more species of animal within whose population the virus is maintained for long periods in relative stability. In other words, the virus circulates at low levels in the population, avoiding the infection of so many individuals that the general population becomes immune to it and the virus has nowhere to go but extinct.
Researchers are getting a pretty good handle on the various mosquito vectors of Zika virus. But we know very little about what animal species act or may act as reservoir hosts for the virus. This information is crucial for understanding the virus’s transmission dynamics and geographical distribution. Without understanding Zika’s reservoir(s) or other hosts, control and prevention will be difficult and inefficient at best, counterproductive at worst.
Probing for a Niche
Numerous mosquito-borne arboviruses have adapted to small mammals or birds as reservoir hosts. These animals in general do not become ill from infection with the virus and are capable of harboring it for extended periods. At least some of the time, these reservoirs have enough virus in their bloodstream to infect a feeding mosquito, allowing the mosquito to transmit the virus to another susceptible host at its next blood meal.
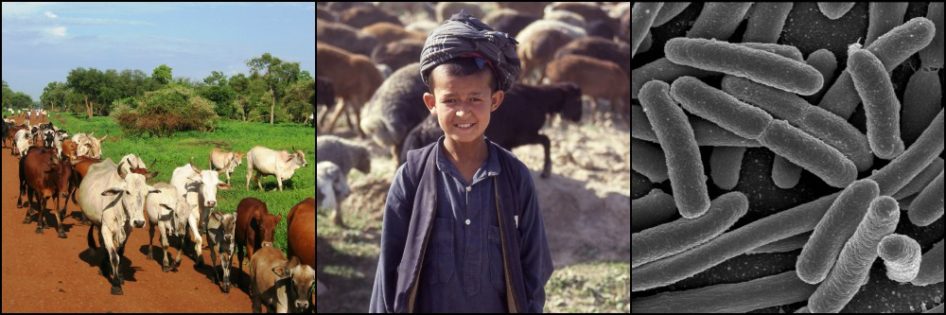
Larger mammals however, including humans and their domestic livestock, tend to serve as dead-end, rather than reservoir, hosts of arboviruses. By definition, thi s means that, when infected, they rarely produce enough virus in their bloodstream to infect a feeding mosquito.
s means that, when infected, they rarely produce enough virus in their bloodstream to infect a feeding mosquito.
In turn, the virus has no evolutionary interest in prolonging the life of a dead-end host because this host is not helping spread the virus’s progeny. As a result, dead-end hosts sometimes, but not always, become very ill and die from the infection, unlike the reservoir hosts.
With Zika virus’s recent arrival to and expansion in the Americas, it is undoubtedly “experimenting” with new vectors and hosts. And unfortunately people are part of this process. Numerous scenarios are possible as the virus discovers what works best for its survival and eventually settles into a relatively stable relationship with reservoir(s) and vectors.
Choosing a Transmission Cycle
A simple human-mosquito transmission cycle is possible, and would not be the worst scenario – for people, at least. In this instance, a focus on control of mosquitoes that feed on humans in affected areas, possibly in conjunction with a vaccination campaign (when a vaccine is finally developed), could eliminate the virus from the Americas.
But the history of other closely related arboviruses suggests this simple human-mosquito cycle is unlikely. Zika virus is a member of the Flavivirus genus, which also includes the closely related viruses that cause yellow fever and dengue fever. Both of these viruses exist in a human-mosquito transmission cycle as described above, with human reservoirs maintaining the virus but generally suffering no ill consequences as a result. This is referred to as an “urban” cycle and occurs in towns and even cities – wherever there are enough people and mosquitoes to keep the cycle going indefinitely.
Why hasn’t the very effective yellow fever vaccine eradicated this disease? Because the urban cycle is not alone. Slightly different forms of both yellow fever and dengue viruses exist in tropical and subtropical forests, independent of the urban cycle and using nonhuman primates as reservoir hosts. These are called “sylvatic” cycles, and occasionally a person who enters these areas, such as to hunt or harvest trees, is infected with a sylvatic virus. These “spillover” infections are typically isolated cases in humans and do not cause outbreaks. In other arboviruses with sylvatic cycles, livestock may also be the victims of spillover infections.
But where effective mosquito control (and vaccination, in the case of yellow fever) have eliminated or significantly curtailed urban yellow fever or dengue cycles, immunity to these viruses has waned in people. This can result in periodic urban outbreaks as the sylvatic virus moves into towns and cities. These outbreaks can be triggered by any number of factors, but usually involve a significant increase in the population of mosquito vectors (see Plague post for a similar mechanism of disease spread).
In these human outbreaks (aka epidemics) caused by the sylvatic yellow fever virus – and apparently also with Zika virus – people become very effective transmitters of the virus to mosquitoes. In this case, people are called amplification hosts because they act as virus factories, fueling the spread of the disease via mosquito bites. But this rapid spread also leads to the virus’s demise, as soon a critical threshold of susceptible people has been infected or is immune and the sylvatic virus must retreat once again into its forest dwelling for lack of potential victims– until conditions are ripe for a new outbreak. As with spillover infections, livestock too may act as amplification hosts for some viruses.

Figure 1. Urban & Sylvatic Transmission Cycles of a Hypothetical Zoonotic Arbovirus
1. Sylvatic Cycle (at left): This involves transmission from mosquito vectors to nonhuman primate reservoir hosts to mosquito…..
2. Spillover Infections (at top): Occasionally, sylvatic virus will infect an exposed, susceptible person or two, such as when clearing virgin forest. These rarely spread, but may cause severe illness.
3. Urban Cycle (at right): virus transmission is from mosquito vectors to human reservoir hosts to mosquito…. Illness in infected persons is rare or mild.
4. Alternative cycles (in red):
A. If the urban cycle is eliminated or suppressed (e.g. through vaccination, mosquito control), sylvatic virus may periodically spread to people in urban areas, causing an epidemic. Infected humans often become ill and spread the virus to biting mosquitoes. The outbreak eventually burns out when enough people have been infected that the virus cannot sustain itself.
B. Occasionally one of these invading sylvatic viruses into an urban area adapts to people and uses them as reservoir hosts, establishing an urban transmission cycle where one did not exist before, or had been eliminated. This is the risk with trying to eliminate Zika virus in people without understanding the virus’s hosts and vectors.
Filling the Void
Hopefully you can see from this explanation that when a sylvatic AND an urban cycle of an arbovirus exists, eliminating the urban cycle may not be enough to prevent human disease. Sylvatic virus may fill the void left by the urban virus.
In the above example, the sylvatic form of the virus abandoned the city when new victims became scarce. But it is also possible that some small genetic changes better adapt the virus to humans, allowing it to remain in urban areas instead of quickly burning itself out there. In this scenario, the virus transitions from using people (or possibly other animals) as amplification hosts to using them as reservoirs, circulating slowly and quietly from one host to another, causing little or no disease.
The RNA genomes of flaviviruses are well suited to rapid genetic changes that can allow this to happen (see avian influenza post for more). And there are closely related precedents. Both Dengue and yellow fever urban cycles are believed to have resulted from changes to the sylvatic cycle viruses hundreds to thousands of years ago that allowed them to move into and maintain themselves in human populations.
Where Does Zika Virus Fit?
We have but few clues to help us predict and search for which animals may be hosts (whether reservoir, dead-end, or amplification hosts) for the Zika virus in the Americas. All information I am aware of is from Africa and Asia and, with one exception, is at least 20 years old (see Table 1 below).
Zika virus was first discovered in 1947 in a rhesus macaque, an Asian monkey used as a laboratory animal in East Africa at the time. This particular macaque was noted to have a fever and, suspecting yellow fever, researchers were surprised to find only an undescribed virus that they named Zika virus, after the Ugandan forest in which they were conducting their research. So from the beginning it was known that Zika can infect at least one nonhuman primate species.
Since then:
- Over one-third of 89 nonhuman primates in the same Zika Forest 22 years later were found to harbor antibodies to Zika virus. Similar antibodies were also found in native nonhuman primates in Senegal in the late 1960s, in Gabon in 1982, and in orangutans in Malaysia in 1996.
- A 2014 study used PCR to identify Zika virus in samples from a grivet monkey from Senegal collected in 1979 and from two rhesus macaque monkeys from Uganda, one collected in 1963 and the other in 1947.
- A study in Pakistan in the early 1980s found antibodies to Zika virus in 1 of 46 domestic sheep, 1 of 48 domestic goats, and a handful of rodents, but none were found in similar numbers of cattle and water buffalo. However, a 1970s study in Indonesia revealed antibodies to Zika virus in an unspecified number of both cattle and water buffalo, as well as bats and domestic ducks, goats, and horses; but not in chickens, rats, or wild birds.

*From a 1968 paper whose contents I have only been able to find reference to.
What does this Information Tell Us?
Unfortunately, not much. It represents only a start to understanding Zika virus hosts. An important caveat is that all but a handful of the positive results for Zika virus in animals are based on the presence of antibodies. These are formed by an animal’s immune system a few days to weeks after exposure to the virus and may remain in the bloodstream for many years after the virus is gone.
Furthermore, the closely related flaviviruses are notorious for cross-reacting with each other on tests that look for antibodies. So it is possible that a previous yellow fever infection in a primate, for example, could result in a “false positive” result for antibodies to the closely related Zika virus. This makes it very difficult to draw conclusions from the small number of studies conducted.
Even if all of the positive results above are correct, the antibody tests tell us only that these animals have been exposed to Zika virus at some point in the past. Whether they were ill from the infection, produced enough virus in their bloodstream to infect mosquitoes, or any other information that might indicate their role as a host to the virus is unknown.
In addition, these studies from the Eastern Hemisphere tell us little about the virus now circulating in South and Central America and the Caribbean. With mounting evidence of birth defects, autoimmune diseases, and possibly other maladies associated with Zika infections in people, the virus that moved across the Pacific islands to Brazil has clearly undergone some changes from the inconspicuous African and Asian viruses from which it once originated.

Figure 2. Current Zika Transmission Worldwide (23 June 2016)
The differences in wildlife species and mosquitoes between Central Africa, Southeast Asia, and the American tropics is significant, making it difficult to predict potential hosts of Zika virus in newly affected areas. European Centre for Disease Prevention & Control
Known mosquito vectors such as Aedes aegypti and the ever-expanding Aedes albopictus are also present in the Americas and, predictably, appear to be competent vectors for the virus there too. But how this American form of Zika virus interacts with a large number of never-encountered wildlife species, in addition to people and livestock, is anyone’s guess.
Birds, which act as the reservoir host for West Nile Virus, another newly arrived flavivirus (see previous post for comparison of Zika and West Nile viruses), are of particular interest. Their hypothetical role as Zika hosts could explain the apparently rapid expansion of Zika virus across South and Central America, and predict further expansion depending on the species of bird involved. But so far we don’t know if birds play any role.
Prospects for the Future
Given the number of nonhuman primates in Africa and Asia in which antibodies to Zika virus have been found, the virus may well settle into a sylvatic cycle in tropical regions of the Americas. Whether infection in people stabilizes at relatively low levels or dies out as more people become immune, or as effective control measures are implemented, will help determine if an urban cycle of Zika is also established.
In any event, the more we know about Zika virus, the more successful and cost-effective efforts will be to control it. The importance of understanding pathogen hosts is highlighted by the example of rinderpest, the devastating cattle disease that was declared officially eradicated in 2011 after a massive, decades-long, international effort. The campaign was nearly halted mid-way through due to the belief that wildlife acted as reservoir hosts and would spread the rinderpest virus back to livestock. Further study, however, showed that when rinderpest was eliminated from livestock, the virus would disappear in surrounding wildlife populations within 4 years. It turned out the livestock were the reservoir hosts in this case, with wildlife for the most part being spillover hosts. The eradication campaign continued and, as predicted, rinderpest disappeared in wildlife soon after it was eliminated from cattle.
Understanding the role played by pathogen hosts is critical to creating practical, realistic plans and expectations. Right now, other than people, we have little idea of Zika virus hosts in the Americas. Hopefully this will soon change.
References
Brès P. Données récentes apportées par les enquêtes sérologiques sur la prévalence des arbovirus en Afrique, avec référence spéciale à la fièvre jaune. Bull World Health Organ.1970; 43(2): 223-267.
Darwish MA, Hoogstraal H, et al. A sero-epidemiological survey for certain arboviruses (Togaviridae) in Pakistan. Trans R Soc Trop Med Hyg. 1983; 77(4): 442-445.
Olson JG, Ksiazek TG, et al. Olson JG Ksiazek TG, et al. A survey for arboviral antibodies in sera of humans and animals in Lombok, Republic of Indonesia. Ann Trop Med Parasitol. 1983 Apr; 77(2): 131-137.
Plourde AR and Bloch EM. A Literature Review of Zika Virus. Emerging Infectious Diseases. 2016 Jul; 22(7).
Vorou R. Zika virus, vectors, reservoirs, amplifying hosts, and their potential to spread worldwide: what we know and what we should investigate urgently. International Journal of Infectious Diseases. 2016 Jul; 48: 85-90.
Weaver SC. (2005). Host range, amplification and arboviral disease emergence. In Peters CJ and Calisher CH (Eds.), Infectious Diseases from Nature: Mechanisms of Viral Emergence and Persistence (pp. 33-44). Austria: Springer.